SUNY Health Network of Excellence targets antibiotic-resistant infections
By Mary Fiess
Over the last 70 years, antibiotics and similar drugs have greatly reduced illness and death from infectious diseases. Many drugs, however, no longer work as well as they once did because the infectious organisms they are designed to kill have adapted to them.
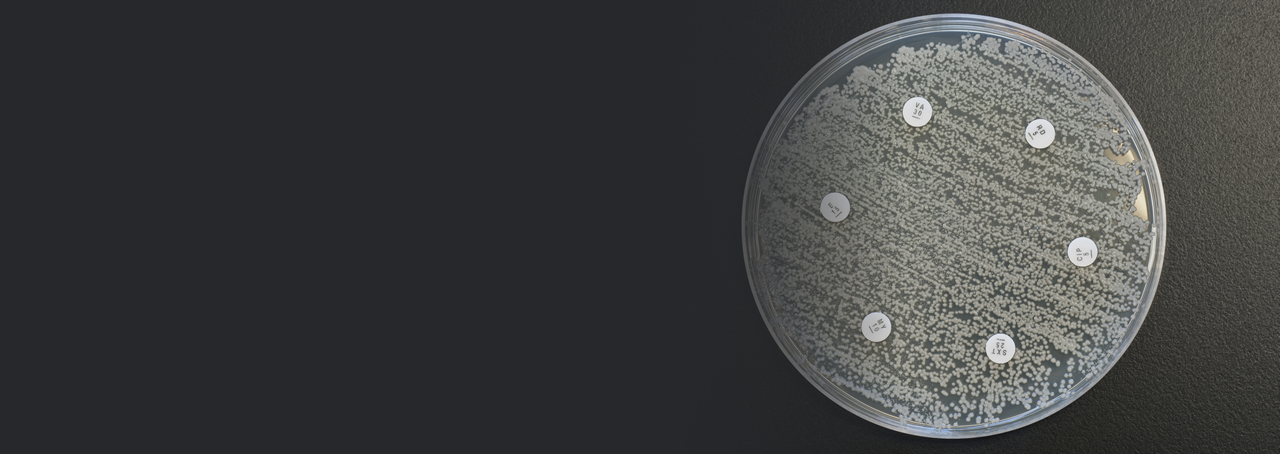
So-called MRSA infections, which are prevalent in hospitals and elsewhere, are one example of the problem. MRSA, methicillin-resistant Staphylococcus aureus, is a type of staphylococcus or "staph" bacterium that is resistant to many antibiotics. Some strains of the bacterium that causes tuberculosis, TB, have also developed antibiotic resistance, making a disease that is already difficult to treat an even greater challenge.
Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die as a direct result of these infections, according to the Centers for Disease Control and Prevention.
This growing public health threat is spurring research to develop new treatments. To advance the work of SUNY researchers in this arena, the SUNY Health Network of Excellence is funding two projects aimed at drug-resistant bacteria, one focusing on the bacterium that causes tuberculosis, Mycobacterium tuberculosis (Mtb), and the other on MRSA.
Leading the project to develop more effective anti-TB therapeutics is Jessica Seeliger, an assistant professor in the Department of Pharmacological Sciences in the School of Medicine at Stony Brook University.
“There are many novel aspects to the bacterium that causes TB that make it difficult to treat. We are particularly interested in the bacterium’s outer membrane and the processes that contribute to its formation,” she says.
“Say you want to build a house and the outer layer is brick. If someone prevented the delivery or assembly of the bricks, your home would be much more vulnerable to damage or destruction. Analogously, we are looking at ways to disrupt the construction of the TB bacterium’s outer membrane and thereby make it more vulnerable,” says Seeliger.
Scientists have long recognized that the structure and composition of Mtb’s cell wall hinder the entry of drugs, making many antibiotics ineffective, but the processes by which the cell wall is formed are not fully understood. By better understanding these processes, Seeliger and her collaborators see an opportunity to develop strategies to inhibit TB infections.
“We are focusing on lipid transport mechanisms. Lipids are molecules that are critical to the formation of Mtb’s outer membrane. We have identified a lipid transport pathway that is required to cause TB infection in animals and is necessary for the transport of one type of lipid – triacylglycerols. We are now doing a series of investigations to characterize the transport protein in this pathway and to identify inhibitors of this protein. Our goal is to extend our studies to elucidate other lipid transport pathways and similarly explore their potential as drug targets,” says Seeliger.
“We hypothesize that inhibiting these pathways will sensitize Mtb to other drugs and/or host defense mechanisms,” she adds.
The project team includes Mahmood Hussain of Downstate Medical Center, G. Ekin Atilla Gokcumen of the University at Buffalo and Eric Rubin of Harvard School of Public Health, who have diverse expertise in mycobacteriology, lipid metabolism, computational methods, structural biology, and infectious disease.
“Tuberculosis kills nearly 1.5 million people around the globe each year,” notes Seeliger. “We hope our collaborative efforts will help develop new strategies to combat this deadly disease and put us in a position to seek and secure further funding to advance our work.”
MRSA, the "staph" bacterium that is resistant to many antibiotics, is the target of a project led by Paul Agris, director of The RNA Institute at the University at Albany. As its name indicates, The RNA Institute focuses on the RNA molecule and ways to harness its features to diagnose and treat disease.
“While DNA contains the multi-step instructions for all proteins, RNA builds proteins using these instructions. RNA controls which proteins are built and their quantities,” explains Agris. “RNA, as a novel therapeutic target for development of new classes of drugs, has the potential to target any step of protein building, including preventing the production of bacterial proteins needed to cause infection.”
In the 1940s, medical treatment for Staphylococcus aureus (S. aureus) infections, commonly known as “staph,” became routine and successful with the discovery and introduction of antibiotic medicine, such as penicillin. In the late 1940s and the 1950s, S. aureus developed resistance to penicillin. Methicillin, a form of penicillin, was introduced to counter the increasing problem of penicillin-resistant S. aureus, but, in 1961, scientists identified the first strains of S. aureus bacteria that had become resistant to methicillin treatment, now known as MRSA. S. aureus continues to evolve and now shows resistance to numerous antibiotics.
“To counter the relentlessly developing pandemic of these multidrug-resistant pathogens, we are taking a new approach that focuses on a family of closely related RNAs as targets for antimicrobial agents,” says Kyla Frohlich, the lead research scientist with Agris at UAlbany. “Our goal is to validate novel drug candidates as a viable new class of antibiotics that kill the MRSA bacterium, but display little-to-no toxicity to human cells.”
“These RNA targets were chosen because they are required for the growth of a large number of bacteria that cause infections, but are not present in humans. This means we could target bacterial RNA and effectively treat a variety of multi-drug-resistant bacterial infections without affecting the human RNA,” explains Frohlich.
Using advanced computer algorithms, 250,000 small molecules were screened for their ability to bind the bacterial RNA target. “We then used this information to conduct experiments in the lab that have identified a potential new antibiotic that kills a wide range of multi-drug-resistant bacteria, including MRSA, and have little to no effect on human cells,” says Frohlich. Patent applications are filed by SUNY RF.
Collaborating with Agris and Frohlich are UAlbany researchers Alan Chen, assistant professor, Department of Chemistry and The RNA Institute, and Kathleen McDonough, research scientist, Wadsworth Center, New York State Department of Health and UAlbany’s School of Public Health; Douglas Kitchen of Albany Molecular Research Inc.; and Paul Kostyniak and Patricia Masso-Welch of the University at Buffalo.
As with the TB project, the team aims to develop new approaches to combatting antibiotic-resistant bacteria, and, says Agris, “we plan to use our findings to support a multi-investigator proposal for funding to the National Institutes of Health.”
comments powered by Disqus